Even though opioids are prescribed by doctors, it’s important to understand their strength. Using them in any way outside of how they’re prescribed—like to relax, sleep, or relieve pain from cramps, migraines, or sports injury—can be incredibly dangerous. Scroll down to learn more about different types of opioids, how they work, and the risks and signs of misusing them.

Click below to learn more about each topic.

The term “opioids” can be a bit confusing because it refers to an entire class of prescription and non-prescription drugs. There are many different types, forms and brands—some you may even be familiar with but never realized contained opioids. Below is a breakdown of the names used most often.

Brands include:
Vicodin®, Lorcet®, Vicoprofen

Brands include:
OxyContin®, Percocet®, Oxecta®, Roxicodone®

It’s often mixed with pain reducers, like Tylenol®, as a prescription

Brands include:
MS Contin®, Oramorph SR, MSIR, Roxanol, Kadian®

Brands include:
ConZip®, FusePaq Synapryn, Rybix ODT, Ryzolt, Ultram®

Brands include:
Methadose®, Dolophine®

Brands include:
Actiq®, Duragesic®, Sublimaze®

Street names include:
Dope, smack, H, junk, skag
Opioids do NOT cure the source of pain. They are strong depressants that bind to receptors in the brain to block pain signals and mask the pain felt in the body. Find out below why this chemical change in your brain can be risky after just a few days.
Prescription pain pills are highly addictive due to their strength, Centers for Disease Control and Prevention (CDC) so they’re only recommended for acute, short-term pain, post-surgery recovery, or for cancer treatment. According to the Centers for Disease Control and Prevention (CDC), they’re not intended for long-term use, chronic pain, or joint and muscle pain.
The CDC states that most pain can be managed in 3 days or less. Using prescription opioids any longer than 7 days is rarely needed, and not effective, as it can lead to opioid use disorder.
Opioids are depressants, which slow down your breathing and heart rate. Too much of the drug in your bloodstream can cause dizziness, lightheadedness, and drowsiness that can give way to breathing problems, falling into a coma, or dying in your sleep.
Chemically, opioids and heroin are almost exactly the same. Both of them attach to receptors in the brain that regulate pain. Because people can become easily addicted to how prescription opioids make them feel, they may seek out a replacement and start experimenting with hard drugs, like heroin, once they run out of pills.
19x
In fact, those who misuse prescription opioids are 19x more likely to start using heroin.
Just because doctors prescribe opioids, doesn’t mean they’re entirely safe. Opioids chemically hijack the brain’s reward system and alter it to crave more and more. Because they’re so addictive, unintentional misuse is incredibly common. Even if your life remains manageable at first, you can become dependent in less than a week.
Opioids don’t just change your brain, they can affect other areas of your life too. At first the changes may be hard to notice, but eventually they build up and can spiral out of control. By learning what to look out for, you can find a way to stop before opioid use turns serious.

Increased irritability and anxiety (especially in between pills); cancelling plans with friends and family; ignoring calls and texts; missing work; and avoiding social interactions.

Putting off responsibilities; being less active; slipping work performance; not taking care of yourself; trouble falling or staying asleep; sleeping at odd hours; and feeling exhausted.

Watching the clock; counting down to your next pill; upping the dosage; constantly thinking about them; taking more often or “just in case;” and using them differently than directed.

Keeping extras on hand; taking pills from friends; needing a dose to function normally; and feeling symptoms of withdrawal (anxiety, rapid heartbeat, nausea, abdominal pain, jitteriness, and vomiting).
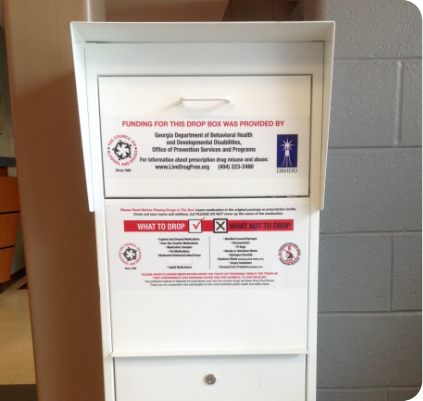
Hanging onto old prescriptions can lead to misuse, especially when stored in a medicine cabinet. Keep yourself and others safe from the temptation to misuse by disposing of leftover pills in a local Drug Drop Box.
180,000
180,000 Georgians have an opioid use disorder.
People you would never expect are accidentally overdosing. In 2019 alone, opioids took 860 lives in Georgia—that’s more than two people every day. The risk of overdose can be much higher for those who have built a tolerance, mix opioids with alcohol or other depressants, or don’t take exactly as directed. Scroll down to learn how to recognize and reverse an overdose.
It can be hard to tell when someone is overdosing because it can look similar to sleeping. Overdoses are caused by having too much of the depressant in their system, which causes their breathing to slow or stop completely. Lack of oxygen flow to the brain can cause brain damage and organ failure. If you notice any of the following signs of overdose, CALL 911 RIGHT AWAY.

A limp or passed out posture and being unresponsive to calls or shakes to wake up.

Pale or clammy face, blue fingernails and lips, or skin color changes (light tones turn to purple and darker tones turn grayish or ashen).
Slow, shallow, or stopped breathing; choking or snoring sounds; or a gurgling “death rattle.”

Slowed or completely stopped pulse, or extreme fluctuations.
Reverse an Opioid Overdose with Naloxone Naloxone (or Narcan®) is the only drug that can reverse the effects of an opioid overdose. When administered through a nasal spray or injection, it can almost instantly restore breathing to normal. Available at most local pharmacies without a prescription, anyone can use this life-saving drug on someone overdosing. Remember to always call 911 as they will still require urgent medical care.


Naloxone (or Narcan®) is the only drug that can reverse the effects of an opioid overdose. When administered through a nasal spray or injection, it can almost instantly restore breathing to normal. Available at most local pharmacies without a prescription, anyone can use this life-saving drug on someone overdosing. Remember to always call 911 as they will still require urgent medical care.


50%
Have naloxone
on hand
as 50% of opioid
overdose deaths
happen at home.
Opioid addiction can happen in just a few days and the longer you use, the more the risk increases. Check out the list of options below that have been proven to manage pain more effectively long-term. Talk with your doctor about other ways of managing pain.
Opioids don’t heal pain or injuries. They’re a short-term way to manage acute pain. If your pain level remains high or continues longer than expected, reach out to your doctor. They can evaluate you to make sure you are healing properly or recommend a treatment that better fits your lifestyle.

